From Bioblast
Description
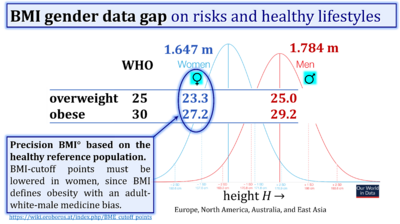
Obesity is defined as a disease associated with an excess of body fat with respect to a healthy reference condition. Cutoff points for body mass excess, BME cutoff points, define the critical values for underweight (-0.1 and -0.2), overweight (0.2), and various degrees of obesity (0.4, 0.6, 0.8, and above). BME cutoffs are calibrated by crossover-points of BME with established BMI cutoffs.
Abbreviation: BME cutoff
Reference: Body mass excess
Events on mitObesity
- 2023 Jun 06: » Health Innovation Summit 2023 Vienna AT
| Healthy reference population | Body mass excess | BFE | BME cutoffs | BMI | H | M | VO2max | mitObesity drugs |
Communicated by Gnaiger Erich 2020-02-15 in: Catastrophe XXX XXX-mass Carol on BME and mitObesity of X-mass Carol
Body mass excess and precision-BMI cutoff lines for overweight and obesity
Calibration of BME cutoff points by BMI crossover points
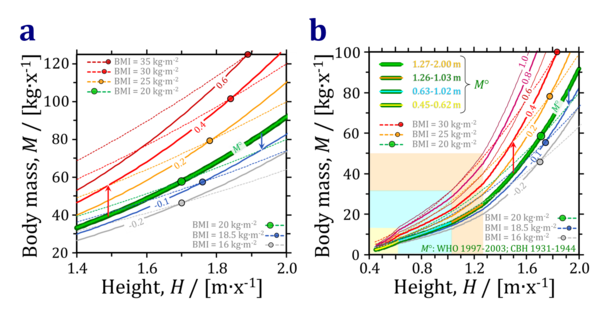
- The healthy reference population, HRP, is characterized by three allometric phases in childhood to early adolescence (up to height 1.26 m/x), and a final phase with an exponent of 2.867 (=1/0.35) at heights above 1.26 m, equal in women and men (Fig. 1; green line for M° at BME=0). Since this exponent is significantly different from 2.0, the body mass index, BMI, predicts a more shallow dependence of body mass on height. The corresponding crossover points — starting with a reference height of 1.7 m/x and normal BMI of 20 kg·m-2 — yield a calibration of BME cutoff points.
- Figure 1: Body mass, M, as a function of height, H, in the healthy reference population, M°, and for specific values of body mass excess, BME (full lines), and crossover with plots of M as a function of H assuming specific values of the body mass index, BMI (dashed lines). The cutoff-crossover point between body mass at BME=0.0 and BMI=20 kg·m-2 (normal) is at 1.7 m/x (green circle). The cutoff-crossover point between body mass at BME=0.2 and BMI=25 kg·m-2 (overweight) is at 1.78 m/x (orange circle). The cutoff-crossover point between body mass at BME=0.4 and BMI=30 kg·m-2 (obese) is at 1.84 m/x (red circle). For body mass at BME=0.6 and 0.8, the corresponding cutoff-crossover points with body mass at BMI=35 and 40 are at 1.89 and 1.92 m/x (not shown). For body mass at BME=-0.1 and -0.2, the corresponding cutoff-crossover points with body mass at BMI=18.5 (underweight) and 16 (severe underweight) are at 1.76 and 1.70 m/x, respectively. At 1.49 m/x the precision BMI of 25 does not indicates obesity instead of overweight (crossover between body mass at BME=0.4 and BMI=25; 1.4M°; vertical arrow upwards). This explains the downwards shift of BMI cutoff-points in Asian populations. At 1.92 m/x the precision BMI of 20 indicates underweight (crossover between BME=-0.1 and BMI=20; 0.9M°; vertical arrow downwards). (a) Height range of 1.4 to 2.0 m/x illustrating the shift of M as a function of BME, indicating underweight (BME = -0.2 and -0.1) or overweight (BME = 0.2) and increasing degrees of obesity (BME = 0.4 and 0.6; full lines). The body mass index, BMI, assumes a more shallow increase of M with H (dashed lines). (b) Four phases of the allometric relationship between M and H in the healthy reference population.
From BMI cutoff points to precision-BMI cutoff lines
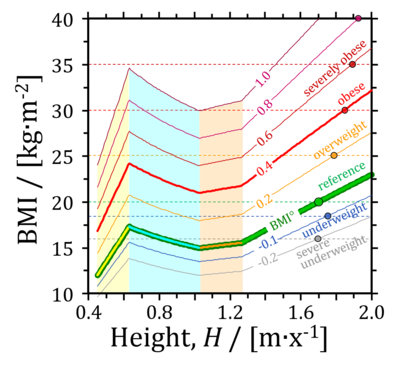
- Figure 2: Comparison of fixed BMI cutoffs (dashed horizonal lines at BMI 16, 18.5, 20, 25, 30 and 35) and precision-BMI cutoffs, BMIx (at BME from -0.2 to +1.0; the numbers x indicate the precision BMIx-cutoff lines), as a function of height in the four phases of the allometric relationship.
- The fixed BMI cutoffs at BMI 18.5 kg·m-2 for underweight, or 25 and 30 kg·m-2 for overweight and obese, do not support a general categorization from children to adults, for women and men, or different ethnic groups. The BME concept resolves these limitations. The BME cutoff is -0.1 for underweight. BME cutoffs are 0.2 and 0.4 for overweight and obese for a large range of ethnic groups including white Caucasians, Black Americans and Asians (Inuit are an exception). Differences in height between Caucasians and Asians explain the limitations of fixed BMI cutoffs. The BME-concept rationalizes the necessary adjustments in the BMI cutoffs for Asians, and thus presents precision BMI-cutoffs (Fig. 2).
References: BMI cutoff points
- - >>>>>>> - Click on [Expand] or [Collapse] - >>>>>>>
| Reference | |
|---|---|
| Cerqueira 2018 Adv Nutr | Cerqueira MS, Santos CAD, Silva DAS, Amorim PRDS, Marins JCB, Franceschini SDCC (2018) Validity of the body adiposity index in predicting body fat in adults: a systematic review. Adv Nutr 9:617-24. |
| Chen 2002 Obes Rev | Chen W, Lin CC, Peng CT, Li CI, Wu HC, Chiang J, Wu JY, Huang PC (2002) Approaching healthy body mass index norms for children and adolescents from health-related physical fitness. Obes Rev 3:225-32. |
| Cole 2000 BMJ | Cole TJ, Bellizzi MC, Flegal KM, Dietz WH (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320:1240-3. |
| Colin 2002 Am J Epidemiol | Colin Bell A, Adair LS, Popkin BM (2002) Ethnic differences in the association between body mass index and hypertension. Am J Epidemiol 155:346-53. |
| Da Silva 2017 Nutrition | da Silva BR, Mialich MS, de Paula FJA, Jordao AA (2017) Comparison of new adiposity indices for the prediction of body fat in hospitalized patients. Nutrition 42:99-105. |
| De Onis 2007 Bull World Health Organization | de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J (2007) Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organization 85:660-7. |
| De Onis 2019 Public Health Nutrition | de Onis M, Borghi E, Arimond M, Webb P, Croft T, Saha K, De-Regil LM, Thuita F, Heidkamp R, Krasevec J, Hayashi C, Flores-Ayala R (2019) Prevalence thresholds for wasting, overweight and stunting in children under 5 years. Public Health Nutrition 22:175-9. |
| Gallagher 2000 Am J Clin Nutr | Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y (2000) Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr 72:694-701. |
| Heymsfield 2014 Am J Clin Nutr | Heymsfield SB, Peterson CM, Thomas DM, Heo M, Schuna JM Jr, Hong S, Choi W (2014) Scaling of adult body weight to height across sex and race/ethnic groups: relevance to BMI. Am J Clin Nutr 100:1455-61. |
| Joshi 2007 JAMA | Joshi P, Islam S, Pais P, Reddy S, Dorairaj P, Kazmi K, Pandey MR, Haque S, Mendis S, Rangarajan S, Yusuf S (2007) Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA 297:286-94. |
| Kuper 2014 BMC Public Health | Kuper H, Taylor A, Krishna KV, Ben-Shlomo Y, Gupta R, Kulkarni B, Prabhakaran D, Davey Smith G, Wells J, Ebrahim S, Kinra S (2014) Is vulnerability to cardiometabolic disease in Indians mediated by abdominal adiposity or higher body adiposity. BMC Public Health 14:1239. |
| Mialich 2014 Nutr Hosp | Mialich MS, Martinez EZ, Jordao JJ (2014) Application of body mass index adjusted for fat mass (BMIfat) obtained by bioelectrical impedance in adults. Nutr Hosp 30:417-24. |
| Mialich 2018 J Electr Bioimp | Mialich MS, Silva BR, Jordao AA (2018) Cutoff points of BMI for classification of nutritional status using bioelectrical impedance analysis. J Electr Bioimp 9:24-30. |
| Misra 2009 J Assoc Physicians India | Misra A, Chowbey P, Makkar BM, Vikram NK, Wasir JS, Chadha D, Joshi Shashank R, Sadikot S, Gupta R, Gulati Seema, Munjal YP, Concensus Group (2009) Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India 57:163–70. |
| Misra 2011 Int J Obes (Lond) | Misra A, Khurana L (2011) Obesity-related non-communicable diseases: South Asians vs White Caucasians. Int J Obes (Lond) 35:167–87. |
| Nevill 2015 Nutr Diabetes | Nevill AM, Metsios GS (2015) The need to redefine age- and gender-specific overweight and obese body mass index cutoff points. Nutr Diabetes 5:e186. |
| Pearson-Stuttard 2018 Lancet Diabetes Endocrinol | Pearson-Stuttard J, Zhou B, Kontis V, Bentham J, Gunter MJ, Ezzati M (2018) Worldwide burden of cancer attributable to diabetes and high body-mass index: a comparative risk assessment. Lancet Diabetes Endocrinol 6:e6-e15. |
| Popkin 2020 Lancet | Popkin BM, Corvalan C, Grummer-Strawn LM (2020) Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet 395:65-74. |
| Romero-Corral 2008 Int J Obes (Lond) | Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, Allison TG, Batsis JA, Sert-Kuniyoshi FH, Lopez-Jimenez F (2008) Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond) 32:959-66. |
| WHO 2000 Sydney Health Comm AU | WHO Regional Office for the Western Pacific (2000) The Asia-Pacific perspective: redefining obesity and its treatment. World Health Organization Western Pacific Region 55 pp. |
| WHO 2006 Acta Paediatr | WHO Multicentre Growth Reference Study Group (2006) WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl 450:76-85. |
| WHO 2006 Geneva: World Health Organization | WHO Multicentre Growth Reference Study Group (2006) WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: Methods and development. Geneva: World Health Organization 312 pp. |
| WHO Expert Consultation 2004 Lancet | WHO Expert Consultation (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363:157-63. |
| Weir 2019 StatPearls | Weir CB, Jan A (2019) BMI classification percentile and cut off points. StatPearls 2019 Dec 7. |
| Wells 2020 Lancet | Wells JC, Sawaya AL, Wibaek R, Mwangome M, Poullas MS, Yajnik CS, Demaio A (2020) The double burden of malnutrition: aetiological pathways and consequences for health. Lancet 395:75-88. |
| Wollner 2017 J Public Health Res | Wollner M, Paulo Roberto BB, Alysson Roncally SC, Jurandir N, Edil LS (2017) Accuracy of the WHO's body mass index cut-off points to measure gender- and age-specific obesity in middle-aged adults living in the city of Rio de Janeiro, Brazil. J Public Health Res 6:904. |
| Xiao 2019 Int J Hypertens | Xiao X, Wang W, Sa R, Qiu L, Liu F (2019) The investigation of sex differences in the effect of body mass index. Int J Hypertens 2019:1360328. |
| Zeng 2014 Br J Nutr | Zeng Q, He Y, Dong S, Zhao X, Chen Z, Song Z, Chang G, Yang F, Wang Y (2014) Optimal cut-off values of BMI, waist circumference and waist:height ratio for defining obesity in Chinese adults. Br J Nutr 112:1735-44. |
Publications: BME and BMI-cutoff
| Reference | |
|---|---|
| Cole 2000 BMJ | Cole TJ, Bellizzi MC, Flegal KM, Dietz WH (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320:1240-3. |
| De Onis 2007 Bull World Health Organization | de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J (2007) Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organization 85:660-7. |
| Gallagher 2000 Am J Clin Nutr | Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y (2000) Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr 72:694-701. |
| Mialich 2014 Nutr Hosp | Mialich MS, Martinez EZ, Jordao JJ (2014) Application of body mass index adjusted for fat mass (BMIfat) obtained by bioelectrical impedance in adults. Nutr Hosp 30:417-24. |
| Mialich 2018 J Electr Bioimp | Mialich MS, Silva BR, Jordao AA (2018) Cutoff points of BMI for classification of nutritional status using bioelectrical impedance analysis. J Electr Bioimp 9:24-30. |
| Romero-Corral 2008 Int J Obes (Lond) | Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, Allison TG, Batsis JA, Sert-Kuniyoshi FH, Lopez-Jimenez F (2008) Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond) 32:959-66. |
| Wollner 2017 J Public Health Res | Wollner M, Paulo Roberto BB, Alysson Roncally SC, Jurandir N, Edil LS (2017) Accuracy of the WHO's body mass index cut-off points to measure gender- and age-specific obesity in middle-aged adults living in the city of Rio de Janeiro, Brazil. J Public Health Res 6:904. |
MitoPedia: BME and mitObesity
» Body mass excess and mitObesity | BME and mitObesity news | Summary |
| Term | Abbreviation | Description |
|---|---|---|
| BME cutoff points | BME cutoff | Obesity is defined as a disease associated with an excess of body fat with respect to a healthy reference condition. Cutoff points for body mass excess, BME cutoff points, define the critical values for underweight (-0.1 and -0.2), overweight (0.2), and various degrees of obesity (0.4, 0.6, 0.8, and above). BME cutoffs are calibrated by crossover-points of BME with established BMI cutoffs. |
| Body fat excess | BFE | In the healthy reference population (HRP), there is zero body fat excess, BFE, and the fraction of excess body fat in the HRP is expressed - by definition - relative to the reference body mass, M°, at any given height. Importantly, body fat excess, BFE, and body mass excess, BME, are linearly related, which is not the case for the body mass index, BMI. |
| Body mass | m [kg]; M [kg·x-1] | The body mass M is the mass (kilogram [kg]) of an individual (object) [x] and is expressed in units [kg/x]. Whereas the body weight changes as a function of gravitational force (you are weightless at zero gravity; your floating weight in water is different from your weight in air), your mass is independent of gravitational force, and it is the same in air and water. |
| Body mass excess | BME | The body mass excess, BME, is an index of obesity and as such BME is a lifestyle metric. The BME is a measure of the extent to which your actual body mass, M [kg/x], deviates from M° [kg/x], which is the reference body mass [kg] per individual [x] without excess body fat in the healthy reference population, HRP. A balanced BME is BME° = 0.0 with a band width of -0.1 towards underweight and +0.2 towards overweight. The BME is linearly related to the body fat excess. |
| Body mass index | BMI | The body mass index, BMI, is the ratio of body mass to height squared (BMI=M·H-2), recommended by the WHO as a general indicator of underweight (BMI<18.5 kg·m-2), overweight (BMI>25 kg·m-2) and obesity (BMI>30 kg·m-2). Keys et al (1972; see 2014) emphasized that 'the prime criterion must be the relative independence of the index from height'. It is exactly the dependence of the BMI on height - from children to adults, women to men, Caucasians to Asians -, which requires adjustments of BMI-cutoff points. This deficiency is resolved by the body mass excess relative to the healthy reference population. |
| Comorbidity | Comorbidities are common in obesogenic lifestyle-induced early aging. These are preventable, non-communicable diseases with strong associations to obesity. In many studies, cause and effect in the sequence of onset of comorbidities remain elusive. Chronic degenerative diseases are commonly obesity-induced. The search for the link between obesity and the etiology of diverse preventable diseases lead to the hypothesis, that mitochondrial dysfunction is the common mechanism, summarized in the term 'mitObesity'. | |
| Healthy reference population | HRP | A healthy reference population, HRP, establishes the baseline for the relation between body mass and height in healthy people of zero underweight or overweight, providing a reference for evaluation of deviations towards underweight or overweight and obesity. The WHO Child Growth Standards (WHO-CGS) on height and body mass refer to healthy girls and boys from Brazil, Ghana, India, Norway, Oman and the USA. The Committee on Biological Handbooks compiled data on height and body mass of healthy males from infancy to old age (USA), published before emergence of the fast-food and soft-drink epidemic. Four allometric phases are distinguished with distinct allometric exponents. At heights above 1.26 m/x the allometric exponent is 2.9, equal in women and men, and significantly different from the exponent of 2.0 implicated in the body mass index, BMI [kg/m2]. |
| Height of humans | h [m]; H [m·x-1] | The height of humans, h, is given in SI units in meters [m]. Humans are countable objects, and the symbol and unit of the number of objects is N [x]. The average height of N objects is, H = h/N [m/x], where h is the heights of all N objects measured on top of each other. Therefore, the height per human has the unit [m·x-1] (compare body mass [kg·x-1]). Without further identifyer, H is considered as the standing height of a human, measured without shoes, hair ornaments and heavy outer garments. |
| Length | l [m] | Length l is an SI base quantity with SI base unit meter m. Quantities derived from length are area A [m2] and volume V [m3]. Length is an extensive quantity, increasing additively with the number of objects. The term 'height' h is used for length in cases of vertical position (see height of humans). Length of height per object, LUX [m·x-1] is length per unit-entity UX, in contrast to lentgth of a system, which may contain one or many entities, such as the length of a pipeline assembled from a number NX of individual pipes. Length is a quantity linked to direct sensory, practical experience, as reflected in terms related to length: long/short (height: tall/small). Terms such as 'long/short distance' are then used by analogy in the context of the more abstract quantity time (long/short duration). |
| MitObesity drugs | Bioactive mitObesity compounds are drugs and nutraceuticals with more or less reproducible beneficial effects in the treatment of diverse preventable degenerative diseases implicated in comorbidities linked to obesity, characterized by common mechanisms of action targeting mitochondria. | |
| Obesity | Obesity is a disease resulting from excessive accumulation of body fat. In common obesity (non-syndromic obesity) excessive body fat is due to an obesogenic lifestyle with lack of physical exercise ('couch') and caloric surplus of food consumption ('potato'), causing several comorbidities which are characterized as preventable non-communicable diseases. Persistent body fat excess associated with deficits of physical activity induces a weight-lifting effect on increasing muscle mass with decreasing mitochondrial capacity. Body fat excess, therefore, correlates with body mass excess up to a critical stage of obesogenic lifestyle-induced sarcopenia, when loss of muscle mass results in further deterioration of physical performance particularly at older age. | |
| VO2max | VO2max; VO2max/M | Maximum oxygen consumption, VO2max, is and index of cardiorespiratory fitness, measured by spiroergometry on human and animal organisms capable of controlled physical exercise performance on a treadmill or cycle ergometer. VO2max is the maximum respiration of an organism, expressed as the volume of O2 at STPD consumed per unit of time per individual object [mL.min-1.x-1]. If normalized per body mass of the individual object, M [kg.x-1], mass specific maximum oxygen consumption, VO2max/M, is expressed in units [mL.min-1.kg-1]. |
MitoPedia concepts:
MiP concept
Labels:
MitoPedia:BME